www.eurowilson.org
Clinical presentation
HOW MAY WILSON DISEASE PRESENT?
Wilson disease may come to light in an individual in a variety of different ways. Indeed, one of the mysteries of this condition is that the same genetic abnormality can produce such different clinical problems in different people.
ASYMPTOMATIC
- When brothers and sisters of a patient with Wilson disease are tested, they are sometimes found to be affected. This usually applies to younger brothers and sisters. Genetic testing can be done immediately after birth.
- If the blood tests which primary care practitioners take in patients with minor illnesses include liver function tests, abnormalities can occasionally be found which on further investigation prove to be Wilson disease
ACTION POINT
If "routine liver function tests" are inexplicably abnormal in a child, test for Wilson disease
HAEMOLYSIS
- Haemolysis can sometime be the first manifestation of Wilson disease, without clinical evidence of liver disease. It may resolve spontaneously, and liver problems may not appear until a year or more later.
- Haemolysis may present simultaneously with liver disease
ACTION POINT
In a child with haemolysis and negative Coombs test, remember to exclude Wilson disease
HEPATIC
The liver manifestations of Wilson disease may be of almost any variety and severity. The important practical message therefore is: suspect Wilson disease in any child with undiagnosed liver disease. Presentations include:
- finding abnormal liver function tests as above, even as early as the first year of life
- finding enlargement of the liver on clinical examination, either in a routine check of an asymptomatic child or during examination of a neurologically affected case.
- an acute hepatitis which appears to resolve. Failure to find a viral aetiology for an acute hepatitis, or delayed or incomplete resolution, should raise the possibility of Wilson disease
- "chronic hepatitis" i.e. continuing abnormality of liver function tests, clinically indistinguishable from an autoimmune hepatitis, though usually not having raised plasma globulin or autoantibodies in the serum
- variceal haemorrhage from unsuspected portal hypertension,
- signs of decompensated chronic liver failure
- fulminant liver failure (FHF). This, the most urgent presentation, causes the most difficulty in diagnosis and management. It usually occurs without antecedent illness but may occasionally be precipitated by an infection. Previous episodes of haemolysis or 'hepatitis' may have occurred.
CLUES suggesting Wilson disease in a child with fulminant liver failure are:
- absence of other known causes
- a relevant family history
- disproportionate rise in bilirubin (>300micromol/l)
- haemolysis on blood film
- relatively low alkaline phosphatase (<600iu/l) or transaminases (100-500iu/l)
NEUROLOGICAL
The neurological manifestations of Wilson disease generally present between the ages of 10 and 35 years; however a patient presenting at 55 years has been published. The neurological manifestations are diverse and may present as movement disorders which can be quite difficult to differentiate from other neurological disorders. They include:
- A dystonic syndrome characterized by dystonic postures and choreoathetosis
- An ataxic syndrome with postural and intentional tremor and ataxia of the limbs
- A parkinsonian syndrome with hypokinesia, rigidity and resting tremor
These three syndromes often occur in the same patient or develop as the disease progresses. Experience in 188 patients (Czlonkowska unpublished data) suggests that the most frequent symptoms are:
- Dysdiadochokinesia (present in all investigated patients)
- Dysarthria (93%)
- Salivation (93%)
- Gait disturbances (79%)
- Postural tremor (wing-beating in 56%)
CLUES suggesting Wilson disease are:
- Wing-beating
- Postural tremor of the arms
- Dystonic posture of the stretched arm behind the back
- Fixed pseudo-smile (risus sardonicus)
- Dysarthria
PSYCHIATRIC
Psychiatric disorders are quite variable. Depression is common. Neurotic behavior includes phobias, compulsive behaviors, aggression, or anti-social behavior. Cognitive deterioration may also occur with worsening school performance, poor memory, difficulty in abstract thinking, and shortened attention span. Pure psychotic disorders are uncommon.
ACTION POINT
Parents' concerns about changes in mood or school performance in a teenager, especially with speech slurring, must be taken seriously. Wilson disease is a rare but possible cause.
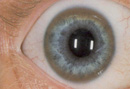
OPHTHALMIC
Usually, the ophthalmologist is asked to look for eye abnormalities in a patientalready suspected of having Wilson disease. Occasionally the optometrist or ophthalmologist may be the first to suspect Wilson disease because of findingthe characteristic eye abnormalities
The Kayser-Fleischer ring is a gold or gray-brown opacity in the peripheral cornea. It first develops superiorly in the cornea (12 o'clock), then inferiorly,and finally in the horizontal meridian. It represents a deposit of copper and sulfur-rich granules in Descemet's membrane, and is reversible with treatment.Additional later ocular findings in Wilson disease include sunflower cataracts,saccadic pursuit movements, loss of accommodation response, and apraxia of opening the eyelid.
RENAL OR SKELETAL ABNORMALITIES
They are very occasionally the first signs of Wilson disease.